Patient experience in 2024: Bridging the gap in patient care journeys
In brief
Data from 6.5M patient encounters explores the state of patient experience today.
- Nationally, things are looking up. Across all settings, we’re seeing patient experience scores rise. In fact, in 2023, ambulatory surgery (85.3 out of 100 top-box “Likelihood to Recommend” rating) and medical practices (84.1) reached a five-year high. Hospital (69.2) and emergency department (66.6) scores have also been on the upswing, but they’ve yet to return to pre-pandemic levels.
- But improvements are neither uniform, nor universal. Underperforming units and departments prove that we need to receive, segment, and analyze data in real time to build on positive momentum.
- Hidden inequities permeate the healthcare system. Patient experiences vary widely based on factors like race, ethnicity, age, gender identity, and location. Underrepresented populations in the inpatient setting face significant disparities in healthcare experiences, particularly around empathy, personalization, and service recovery. And these gaps are exacerbated in medical practices, with the largest gap (7 points) separating Asian and White patients’ scores. To achieve true equity, organizations must understand where these differences exist—and why.
- Millennial and Gen Z patients are being left behind. Younger generations consistently report lower PX scores than their predecessors—for example, a 7.7-point gap in “Likelihood to Recommend” (LTR) separates patients age 18–34 and those 65–79. One reason? Millennials and Gen Z patients have higher expectations around access and less tolerance for friction, and they want more information about conditions, medications, and treatments.
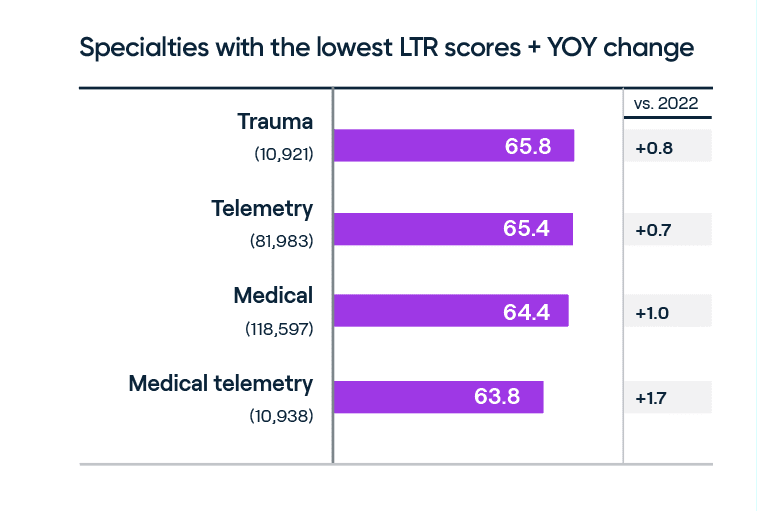
- Unplanned admissions rank lower in PX. Specialties where planned admissions are the norm, like cardiac surgery and obstetrics, boast higher patient loyalty and LTR than unplanned admissions (like trauma). Effective communication, a key driver of patient experience, is typically more seamless in planned care, leading to clearer patient expectations and a better sense of outcomes.
- West and South-Central are outperforming in PX. Regions that once had the most room for improvement are now making the greatest strides. Looking at scores at a state-by-state level, Nevada jumped +2.3 points to 78.5, continuing its reign as the top state for patient experience. But Arkansas edged its way into the top five this year, despite its modest +0.9-point gain (to 74.0), demonstrating that even small shifts can have significant outcomes.
Healthcare is a deeply personal journey. Every individual has unique needs, expectations, and perspectives. And whether or not those are acknowledged can be the difference between a positive, healing experience, and one that may leave room for uncertainty.
But how do we, as experience leaders, put our best foot forward? How do we improve the patient experience, when PX isn’t homogeneous, and each person comes from different backgrounds, with different emotions and concerns? It starts with empathy, with gratitude, and with love. These are the threads that pull people together, create a sense of belonging, and connect us in a world that can often feel fragmented. Achieving this starts with listening to each other, so we can better understand each other. By listening to patients and understanding the patient experience (PX), we gain valuable insights into how we can create a more positive healthcare journey for everyone.
In today's hyper-competitive healthcare landscape, delivering exceptional patient experiences isn't just a nice-to-have—it's a necessity. Press Ganey’s report “Patient experience in 2024” analyzes data from 6.5M patient encounters across the U.S. to better understand the state of patient experience today, as well as opportunities for improvement moving forward. And, after several volatile years, the data finally brings us some good news: PX is rebounding from COVID-19 declines, and scores at some institutions are even hitting record highs.
While national trends show signs of promise, pain points around safety, equity, and personalization are still impacting the patient experience. To improve PX and elevate the experience for all, organizations must identify where gaps exist—and for whom. In doing so, we can bring everyone in the industry back from pandemic-induced challenges, and press forward toward a new, more promising horizon in health, care, and Human Experience.
Decoding the patient experience: Improvements and opportunities
Patients reported more positive perceptions of their care in 2023 compared to the previous year, with scores in ambulatory surgery and medical practices hitting five-year highs (85.3 and 84.1 out of 100, respectively). While hospitals and emergency departments are improving too, they haven’t yet fully recovered to pre-pandemic levels. There’s more good news: Most settings, aside from ambulatory, where LTR scores are plateauing, are continuing to see growth, and we expect them to similarly reach record highs later this year.
But a deeper analysis shows that disparities persist by region, demographic, and care setting. This means a one-size-fits-all approach to improving patient experience has inherent limitations. Organizations must segment their data to truly understand the experiences of all patients, regardless of who they are, what their needs are, or where they seek care.
Analyzing PX scores based on race and ethnicity
Racial and ethnic inequities continue to undermine the health and well-being of our communities. This difference, called the “experience gap,” is measured by the difference between the highest- and lowest-scoring groups.
In the inpatient setting, PX trends for some racial and ethnic groups are looking more favorable, but there's still much room for improvement. These opportunities vary by demographic, care setting, and patient experience issue.
Generally, White patients report slightly higher-than-average scores (though it’s important to note that they represent the majority of respondents). Those identifying as Spanish/Hispanic/Latino and Native Hawaiian/Pacific Islander also rate experiences higher on most measures.
Other key takeaways include:
- Black/African American patients report worse-than-average experiences around staff teamwork, empathy, and privacy.
- American Indian/Alaska Native report more negative experiences for most elements of care, aside from certain aspects related to information and amenities.
- Despite relatively higher scores overall, Hispanic/Latino and Native Hawaiian/Pacific Islander patients report lower experiences around the courtesy of room cleaning services. Native Hawaiian/Pacific Islander also report more negative experiences around attention to their needs.
In the medical practice setting, these equity gaps are even more pronounced. The biggest experience gap for “Likelihood to Recommend” is between Asian and White patients, with the former scoring 6.3 points lower, and the latter 0.7 points higher, than average.

Generational divides in patient experience scores
Younger generations—i.e., millennials (born 1981–1996) and Gen Zers (1997–2012)—report lower PX scores than boomers (1946–1964). We can, perhaps, attribute this to the rising expectations around convenience and access of these digital-first generations, who are more discerning healthcare consumers, have less brand loyalty, and are more likely to “shop around” for care.
While, admittedly, all generations have seen modest improvements in LTR, younger patients score the lowest: 77.7 among 18–34-year-olds vs. 80.3 for 35–49-year-olds and 85.1 for 65–78-year-olds. But as millennials increasingly step into caregiver roles—not just for themselves, but for children and/or aging parents—and Gen Z starts taking a more active role in their healthcare decisions, organizations must rethink their strategies to reach these younger patients, now in the driver’s seat.
Patient experience variations by specialty and care setting
PX scores across most specialties are steadily improving, as pandemic-induced fluctuations stabilize, and the industry gets back on track. Notably, patients express higher loyalty in specialties related to planned patient admissions, where care is coordinated, and patients benefit from presurgical preparation, consistent communication, and reliable post-discharge support. Conversely, unplanned admissions tend to see lower LTR scores.

Location, location, location: PX variation by region
A 13.8-point gap separates the top- and bottom-performing states. Nevada, which saw a huge, +2.3 jump in PX scores YOY, continues to lay claim to the #1 spot for patient experience (78.5). New to the top five this year is Arkansas, which jumped +0.9 points to 74.0. Seemingly small shifts in scores can have a huge impact on rankings.
The top 10 states for patient experience in hospitals*:
- Nevada (+2.3 to 78.5)
- North Carolina (+1.2 to 74.9)
- New Mexico (+0.5 to 74.5)
- Ohio (+0.3 to 74.2)
- Arkansas (+0.9 to 74.0)
- Washington (+0.2 to 74.0)
- South Dakota (+0.5 to 73.9)
- Alabama (+0.0 to 73.3)
- New York (+1.7 to 73.2)
- Utah (+2.0 to 73.2)
*States where Press Ganey has 7 or more clients for statistically stable data.
While overall patient experience has improved, the Midwest and West (American Hospital Association, or AHA, regions 6–9) demonstrate higher scores compared to the Northeast, Mid-Atlantic, and South-Atlantic (AHA regions 1–3). AHA region 2 (New Jersey, New York, and Pennsylvania) saw the most significant growth, (+1.8 YOY)—more than doubling the rate of improvement (+0.7) of AHA region 7 (Arkansas, Louisiana, Oklahoma, and Texas), which led the nation in patient experience (72.9) in 2023.
The bottom line: Taking a “one size fits all” approach to patient experience improvement falls short
Healthcare is constantly evolving. New technologies and innovations drive better care delivery and outcomes. And new patient expectations have set a higher bar for their experiences—not just within your “four walls,” but before and after each episode of care.
That said, what was always important to patients is still important to patients—possibly even more so. And these typically have everything to do with healthcare employees and their interactions with patients. Employee experience and patient experience are tightly intertwined. In fact, facilities that score at the top for employee engagement are 3x more likely to perform at the top in patient experience too.
The top drivers of inpatient LTR scores have remained remarkably stable over the past five years:
- Staff worked together to care for you
- Response to concerns/complaints
- Attention to needs
- Nurses’ attitude toward requests
- Nurses kept you informed
In moments of vulnerability and uncertainty, individuals often yearn for and seek out meaningful human connections. As healthcare professionals, we’re not just treating ailments or injuries, diseases or conditions. We’re caring for people. We’re caring for our communities. And we’re caring for each other.
So, how do we, as individuals and as an industry, make meaningful improvements we can sustain over the long term?
1. Expand listening across the care journey. Understanding the patient journey is crucial to delivering exceptional care. By establishing robust feedback loops, healthcare organizations can gain invaluable insights into patient experiences and needs. From the moment a patient starts looking for care to post-discharge and beyond, capturing feedback through digital interactions, social media, review sites, and more provides a comprehensive, 360° view of their journey. This continuous listening process is essential for identifying pain points, addressing concerns, and, ultimately, improving outcomes.
2. Delve deeper than national benchmarks by analyzing performance at the regional, local, facility, unit, and specialty levels. In today’s hyper-competitive healthcare landscape, tracking patient experience performance is essential. While national benchmarks are critical, and provide a valuable starting point, a deeper understanding of local trends is also crucial for gaining a competitive edge.
3. Bring patients and their families into decision-making. On a macro level, creating advisory groups that elevate these voices helps healthcare organizations gather qualitative feedback while nurturing a sense of community inclusion. Scaling down, it helps organizations better understand the individuals they are caring for directly. Digital tools let organizations do this faster, and more accurately, and tune in to a wider array of diverse voices—leading to more inclusive decision-making.
4. Maximize impact through data-driven insights and interventions. Segmenting patient experiences and identifying trends can pinpoint areas for improvement with more precision than ever before. Leveraging AI and natural language processing, organizations can analyze vast quantities of quantitative and qualitative patient feedback to uncover actionable insights, prioritize at-risk patient populations, and develop targeted solutions to improve the patient experience, for all.
5. Embrace technology as a “member” of the team. In an era of limited healthcare teams and resources, technology can be a critical ally in the ongoing pursuit of better experiences and outcomes. Care teams can optimize their workflow through tools designed to streamline daily tasks. For example, predictive rounding technology can identify patients in need of immediate attention. The strategic use of follow-up communications can significantly improve patient adherence to post-discharge care plans—ultimately reducing readmission rates and elevating the overall patient experience.
Download our report, “Patient experience in 2024,” to see all findings and recommendations from our recent study. To discuss the data—and its implications for your organization—reach out to a member of our patient experience team.